Respiration is defined as the flow of oxygen from the outside into the cells and tissues and transport of carbon dioxide to the outside environment. The respiratory system works collaboratively with the cardiovascular system for proper gas exchange between the cells and blood. The inability for the respiratory system of a child to supply oxygen or remove carbon dioxide can cause low blood oxygen or hypoxemia or high blood carbon dioxide or hypercapnia; resulting in respiratory problems and failure.
Recognizing the signs and symptoms of various respiratory problems and shock especially in an ill or injured child is critical in preventing cardiopulmonary failure and cardiac arrest. Cardiac arrest in infants and children is usually a result of continuous respiratory failure, shock or both and the survival rate for these kids is really low. Understanding and knowing the proper interventions and assessment techniques is crucial to prevent further damage. The pediatric advanced life support (PALS) provides a systemic approach in assessing and treating an ill or injured child due to respiratory distress, respiratory failure and shock to prevent further deterioration and death.
The American Heart Association in conjunction with the American Academy of Pediatrics recommends an evaluation model and an assessment technique which is used to provide health care professionals with the tools and techniques needed to adequately treat pediatric patients in respiratory distress, failure or shock. The evaluation model to treat a seriously ill or injured child is the “assess-categorize-decide-act” model. The first part of the model is the assessment part and there are four assessments to the systemic approach:
The general assessment is the first part to of the evaluation process that requires a quick visual and auditory assessment of the child at risk and looks for appearance, breathing and circulation. A deficient in any of the following categories indicates an underlying problem or illness that requires immediate attention and treatment.
Primary Assessment
Upon the completion of the general assessment which requires a quick visual and auditory observation, the primary assessment is activated. The primary assessment is a thorough, hands-on, cardiopulmonary and neurological evaluation of the child, which uses the ABCDE approach. Vital signs and oxygen saturation are analyzed during the primary assessment.
ALWAYS REMEMBER TO WATCH OUT FOR LIFE-THREATING PROBLEMS THROUGHOUT THE ASSESMENT TO ENSURE THEY ARE TREATED AS THEY ARISE
A = Airway
Ensure the airway is patent, meaning it’s open and unobstructed, and is able to be maintained by normal methods or by advanced interventions. Look for movement of chest and listen and feel for air movement and sounds. Upper airway obstruction can be noted if the patient has restricted inspiratory effort, there are abnormal or no breath sounds.
B = Breathing
Breathing is when air moves in and out of lungs and is measured by the following:
Respiratory rate is indicated as the number of breaths over a period of time for both adults and children. Respiratory rate may vary due to different reasons such as fever, anxiety, exercise, pain, excitement or other medical conditions. The following chart shows normal and abnormal respiratory rate in children, respiratory effort, tidal volume, airway and lung sounds, and pulse oximetry.
| Normal Respiratory Rate | Abnormal Respiratory Rate |
| Depends on age = 12-60 bpm Infant (< 1 yr) 30-60 bpm Toddler (1 to 3 yrs) 24-40 bpm Preschooler (4 to 5 yrs) 22-34bpm School age (6 to 12 yrs) 18-30 bpm Adolescent (13 to 18 yrs) 12-16 bpm |
Tachypnea – >60 bpm at any age (always abnormal) Bradypnea – <20 bpm from ages 3-12 years Apnea – no breathing |
| Normal Respiratory Effort | Abnormal Respiratory Effort |
| Normal effort with air moving in and out | Nasal flaring, chest retractions, head bobbing or seesaw respirations |
| Normal Tidal Volume | Abnormal Tidal Volume |
| 5 to 7 milliliters/kilogram of body weight | Decreased or asymmetric chest expansion and distal air movements |
| Normal Airway & Lung Sounds | Abnormal Airway & Lung Sounds |
| Soft, quiet inspiratory sound Short, quieter or absent expiratory sound |
Stridor, grunting, wheezing, gurgling or crackle sounds |
| Normal Pulse Oximetry | Abnormal Pulse Oximetry |
| Oxygen Saturation ≥94% | Oxygen Saturation ≤94% |
C = Circulation
The next part of the assessment is circulation. Circulation includes cardiovascular function and end-organ function. Proper cardiovascular function is seen through the following:
Proper end-organ function is seen through the following:
The following table shows the normal and abnormal of circulation in a child:
| Normal Skin Color & Temperature | Abnormal Skin Color & Temperature |
| Consistent over trunk and extremities Nail beds, palms and soles of feet should be pink |
Hands, feet, trunk and extremities turn pale, cool and mottled. Hands, feet and periphery will be affected first |
| Normal Heart Rate | Abnormal Heart Rate |
|
Depends on age of child: |
Tachycardia – faster than the normal range for the child’s age Bradycardia – slower than the normal range for the child’s age |
| Normal Heart Rhythm | Abnormal Heart Rhythm |
| Regular with small fluctuations in rate | Loss of peripheral pulses and weak central pulses |
| Normal Blood Pressure | Abnormal Mean Arterial Pressure (mm Hg) |
| Depends on age of child |
Newborn < 45 mm Hg Infant/Toddler > 50 mm Hg Preschooler < 58 mm Hg School-age child < 66 mm Hg Adolescent < 71 mm Hg |
| Normal Pulses | Abnormal Pulses |
| Easy palpitation of central and peripheral pulses | Loss of peripheral pulses then weakening central pulses |
| Normal Capillary Refill Time | Abnormal Capillary Refill Time |
| < 2 seconds | >2 seconds due to dehydration, hypothermia and shock |
| Normal Brain Function | Abnormal Brain Function |
| Score of 15 on Glasgow Coma Scale (GCS) | Cerebral hypoxia results in loss of muscular tone, seizures, papillary dilation and unconsciousness. A score of <15 GCS; no response or lack of spontaneity in response. |
| Normal Skin | Abnormal Skin |
| Pink and consistent over trunk and extremities | Petechia, pupura, cyanosis, pallor and mottling |
| Normal Renal Perfusion | Abnormal Renal Perfusion |
| Adequate urine output dependent on age Infants and young children: 1.5-2 mL/kg/hr Older children and adolescents: 1 mL/kg per hour | Low urine output below the range for the child’s age |
| Normal Glasgow Coma Scale | Abnormal Glasgow Coma Scale |
| Eye opening: spontaneous, Best motor response: obeys commands Best verbal response: oriented | No response or lack of spontaneity in response |
| Normal Hypoglycemia | Abnormal Hypoglycemia |
| >40 mg/dL in newborn | <40 mg/dL in newborn |

Secondary Assessment
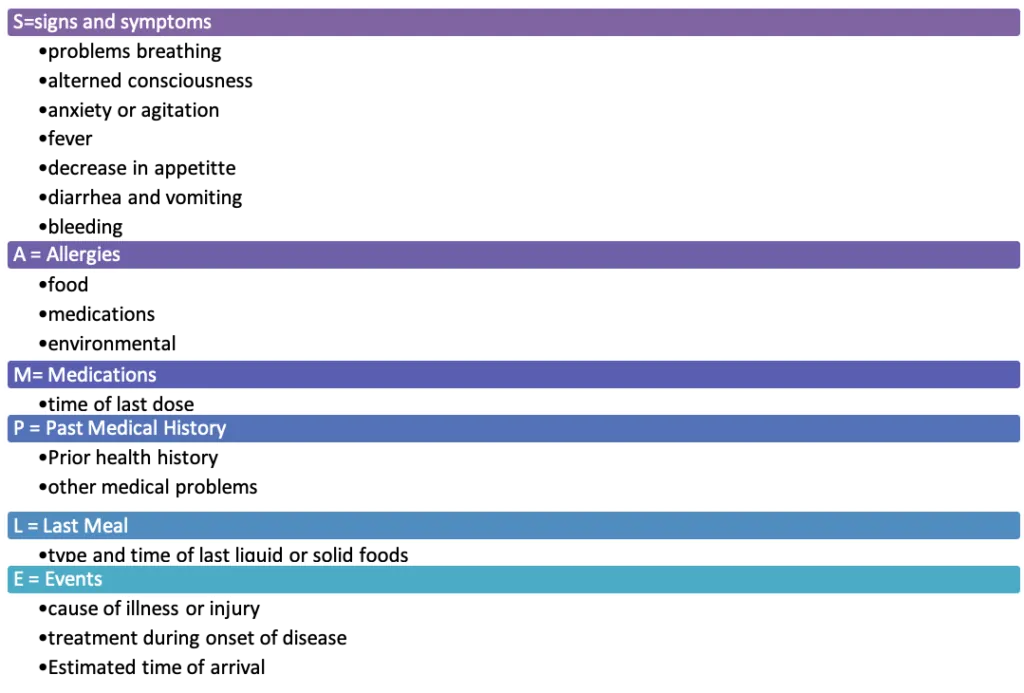
After the completion of the primary assessment, the secondary assessment should be performed by obtaining a more in depth history and conducting a thorough physical exam. During the secondary assessment the SAMPLE mnemonic is used to help with the evaluation process.
Tertiary Assessment
The tertiary assessment is used to find the cause and problems associate with respiratory and circulatory systems. This evaluation process uses both laboratory and nonlaboratory studies to help detect these problems. Laboratory or blood studies show, arterial blood gas (ABG), venous blood gas (VBG) and hemoglobin concentration. The nonlaboratory studies include: pulse oximetry, exhaled CO2 monitoring, capnography, chest x-ray, and peak expiratory flow rate.