Video Demonstration
Ventricular Fibrillation and Pulseless VT (Part 1)
Ventricular Fibrillation is a life-threatening arrhythmia which can lead to sudden cardiac arrest. During VF, there is no organization of electrical activity in the heart and the cardiac muscle is in irregularity and disarray. This rapid and unorganized fluttering of the heart leads to inadequate blood pumped through the systemic or pulmonary circulation, leading to an irregular heart rate. VF can turn into asystole, or sudden cardiac death, in a matter of minutes.
Ventricular Fibrillation and Pulseless VT (Part 2)
Ventricular tachycardia (V-tach or VT) is a fast heart rhythm from the ventricles of the heart. VT can lead to VF and cause sudden death of the patient. A pulseless VT has no cardiac output causing no pulse and results in cardiac arrest. Ventricular fibrillation (VF) is an arrhythmia, which can cause sudden cardiac arrest. During ventricular fibrillation there is irregular organization of electrical activity in the heart. VF has many causes:
Symptoms of VF include:
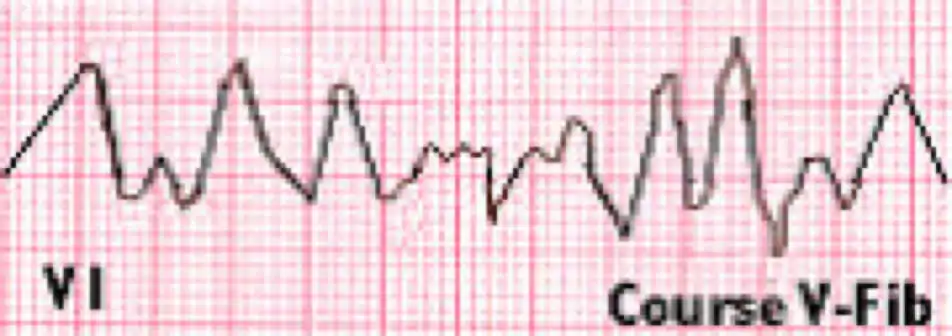
VF does not have an identifiable ECG waveform. Earlier waveforms show a “coarse VF,” but after few minutes the waveforms are much smaller and show a “fine VF.”

Pulseless Ventricular Tachycardia
Ventricular tachycardia (V-tach or VT) is a fast heart rhythm from the ventricles of the heart. VT can lead to VF and cause sudden death of the patient. A pulseless VT has no cardiac output causing no pulse and results in cardiac arrest. The causes of pulseless VT are:
The symptoms of pulseless VT are similar to that of VF and follow the same treatment protocol.

This section will cover assessment, intervention, and management of an adult with VF or pulseless VT where the abnormal rhythm is recurrent or did not respond to the first shock. Instead of using the AED, a manual defibrillator will need to be used. The management of VF, pulseless VT, ECG artifact that resembles VF and New left bundle branch block will be covered. Management of these cardiac rhythms will require the efforts of a full team.
A resuscitation team includes the following:
Let’s take a look at a scenario.
Scenario: You are on-call at the ER and you see a man running towards you and all of a sudden you see him fall to the ground. You rush over there and notice that the man is holding his chest and is having difficulty breathing. After few seconds he loses consciousness.
Assessment:
Interventions:
Management: Initiate the cardiac arrest algorithm if the patient still has no pulse and does not respond to BLS.
We will look at the Cardiac Arrest Algorithm in the following chapter.
Learning Outcomes:
You have completed Chapter VIII. Now you should be able to: