Stroke is one of the leading causes of deaths in the United States. Over 700,000 people suffer from acute stroke medical emergencies every year in the US and 1/6 cardiovascular deaths are stroke related. Early detection of a patient having stoke is important because they will need IV fibrinolytic treatment within 3 to 4.5 hours of the initial symptoms.
Acute Stroke
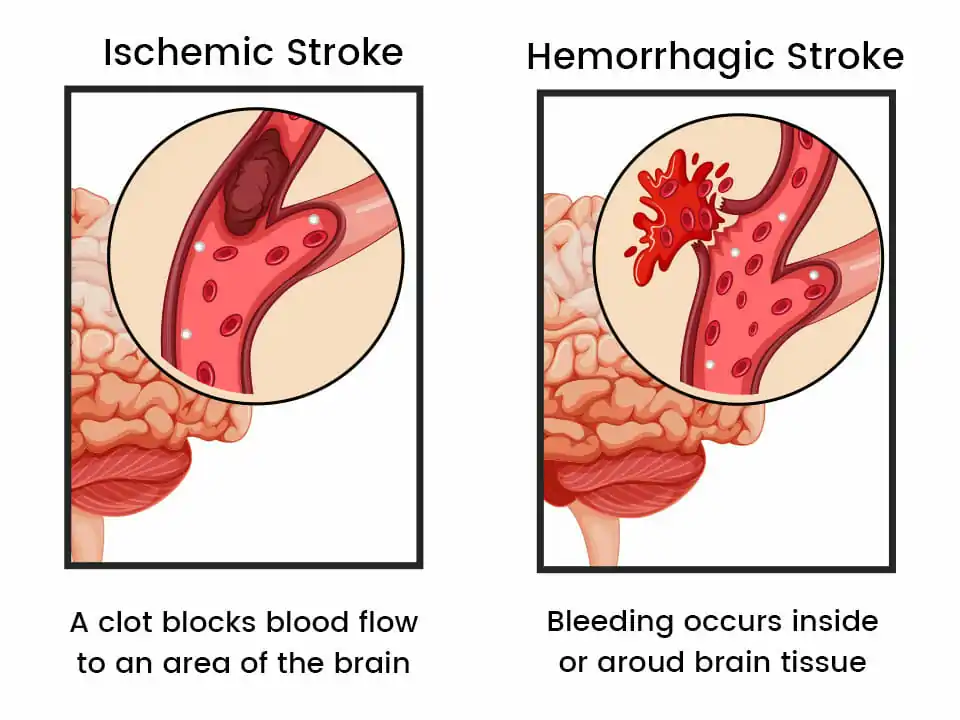
Understanding the signs of a suspected stroke and fastened response helps save patient’s life while maintaining its quality. Stroke occurs due to insufficient blood flow to the different area of the victim’s brain. There are 2 major ACLS stroke types:
Adequate ACLS stroke care involves reducing brain injury and increasing chance of patient’s recovery. According to the American Heart Association (AHA) there are 8D’s of stroke care, important in diagnosis and treatment of a stroke.
| Detection: Rapid recognition of stroke symptoms |
| Dispatch: early activation and dispatch of EMS by 911 |
| Delivery: Rapid EMS identification, management, and transport |
| Door: appropriate triage to stroke center |
| Data: Rapid triage, evaluation, and management within ED |
| Decision: Stroke expertise and therapy selection |
| Drug: Fibrinolytic therapy, intra-arterial strategies |
| Disposition: Rapid admission to the stroke unit or critical care unit |
Reference: American Heart Association. Advanced Cardiac Life Support (ACLS) Student Provider Manuel. Dallas: American Heart Association, 2011. Print
Stroke Chain of Survival
Possibility of permanent brain damage and risk of death reduces with the chain of survival. It is:
The Cincinnati Prehospital Stroke Scale from strokecenter.org highlights ways in recognizing accurate symptoms of a stroke.
Facial Droop
Arm Drift
Speech
|
If any 1 of these 3 signs is abnormal, the probability of a suspected stroke is 72%. The presence of all 3 findings increases probability of a stroke to >85%
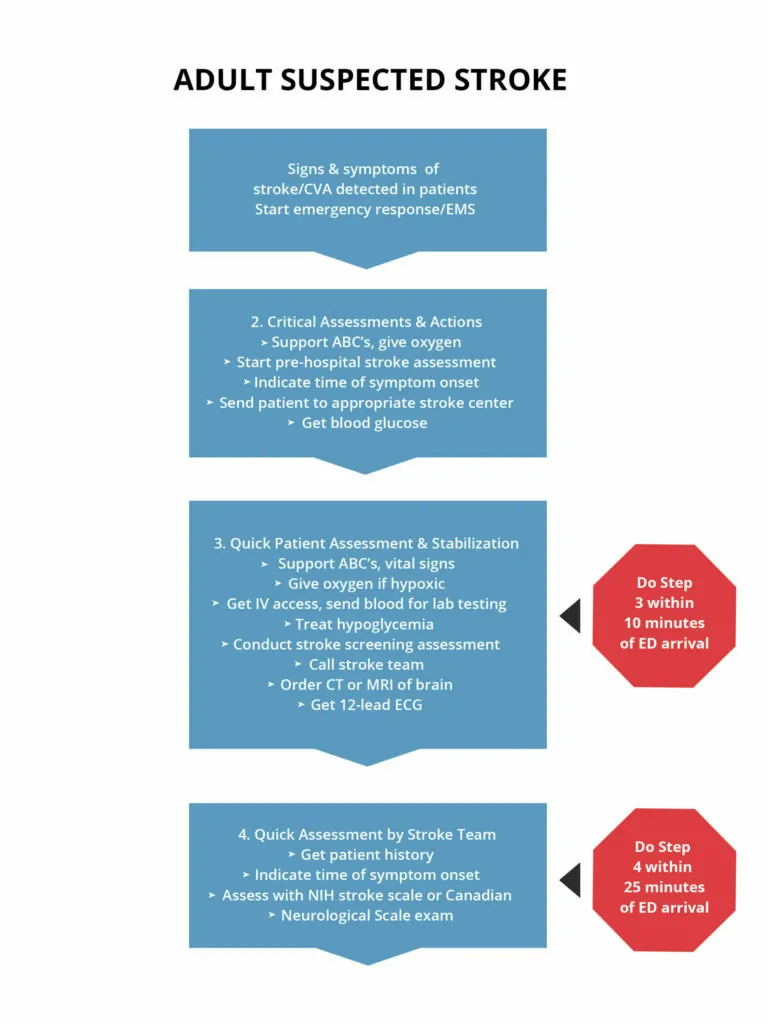
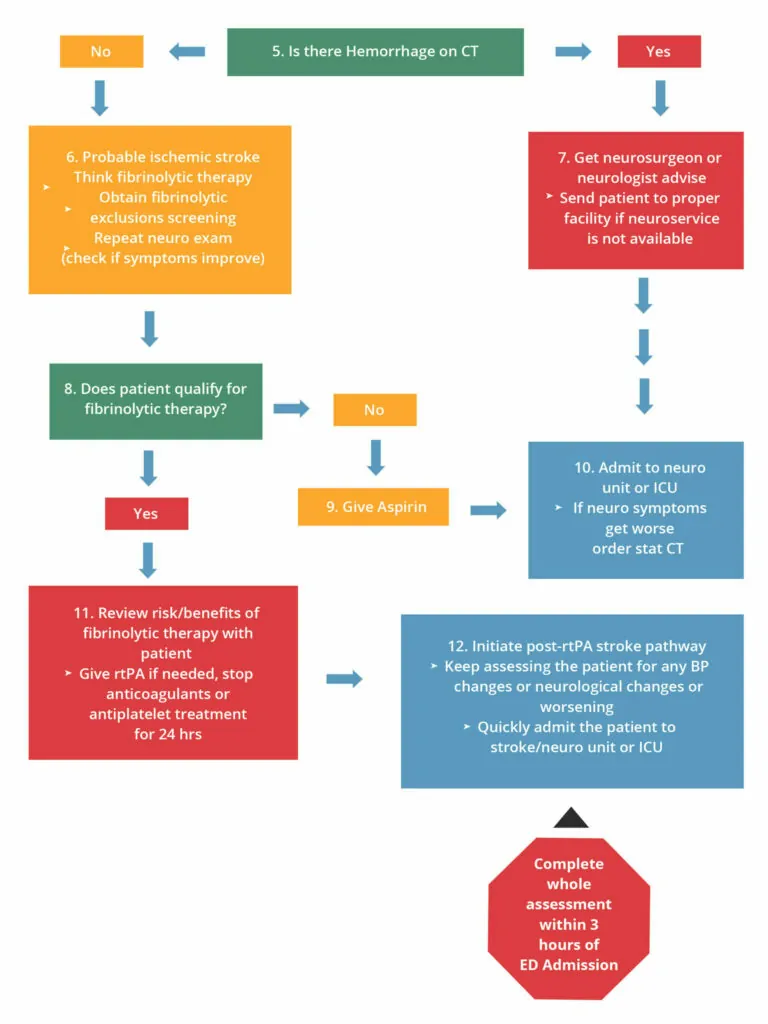
The following is an algorithm showing management of acute stroke:
Treatment of Stroke Patients Goals
CT scan Interpretation
The purpose of the CT scan is to differentiate between ischemic and hemorrhagic stroke. The most common type is a non-contrast CT scan for the acute stroke patient. Treatments for hemorrhagic and ischemic stroke are:
Fibrinolytic Therapy
The NINDS protocol and criteria show tPA is the first line treatment within 3 hours of the onset of symptoms for patients who have acute ischemic stroke. The AHA guidelines recommend IV tPA administration for patients with acute ischemic stroke. To qualify a patient for fibrinolytic therapy a checklist must be applied.
| Inclusion Criteria (all below should be YES) | Exclusion Criteria (all below should be NO) | Relative Contraindications /Precautions |
|---|---|---|
| Patient is 18 years or older? | Intracranial hemorrhage on non-contrast head CT? | Symptoms are not major and improve quickly and spontaneously |
| Dx of ischemic stroke with neurologic deficit? | Presentation of patient shows subarachnoid hemorrhage even with normal CT? | 14 days since major surgery or trauma |
| Time of system onset – less than 3 hours? | Multilobar Infarction on CT (hypodensity greater than 1/3 of cerebral hemisphere)? | Current GI or Urinary tract hemorrhage (approx. 21 days) |
| All ABOVE SHOULD BE YES | History of intracranial hemorrhage? | Current acute Myocardial infarction (in approx.. 3 months) |
| Hypertension: SBP > 185 mmHg or DBP > 110 mm Hg on repeated measurements? | Postmyocardial infarction pericarditis | |
| Arteriovenous malformation, neoplasm, or aneurysm? | Abnormal blood glucose level (400 mg/dl [22.2 mmmol/L]) | |
| Witnessed seizure at stroke onset? | THESE ARE ALL CONTRAINDICATIONS /PRECAUTIONS | |
| Active internal bleeding or acute trauma (fracture)? | ||
Acute bleeding diathesis, including
|
||
| History of intracranial or intraspinal surgery, serious head trauma or previous stroke within past 3 months? | ||
| Arterial puncture at a noncompressible site within past 7 days? | ||
| ALL ABOVE SHOULD BE NO! |
Learning Outcomes:
You have completed Chapter XIII. Now you should be able to: